The more accurately the health data is shared across the clinic operations, the better care services the medical staff can provide. It’s more than just connecting healthcare software – it’s about creating a smooth, secure flow of patient data between systems, departments, and providers. That’s where EHR integration comes in to improve workflows and benefit the quality of care.
List of the content
- What is EHR integration?
- How to perform EHR integration?
- Challenges of electronic health record integration
- 5 reasons to start EHR integration
- Conclusion
What is EHR integration?
This process connects the clinic’s Electronic Health Record (EHR) system with other healthcare systems, software, or devices to facilitate the secure and accurate sharing of data. It allows care providers to integrate various tools that share data with each other and support real-time updates of patient health data.
The medical staff no longer needs to transfer health records manually. Moreover, they don’t re-enter data in multiple places, as it is instantly shared across all connected solutions. For example, when a patient’s lab test result is available, it appears instantly in their profile for the practitioners’ review. Health records reflect all these changes and make updates available to authorized users. And the data exchange can save time and support safer and faster decisions throughout the patient care journey.
Therefore, EHR integration provides a centralized and automated method for accessing complete and up-to-date health records. The result is a more connected healthcare environment with a well-arranged information flow. Clinics get more improved decision-making, fewer errors, and better patient experiences.
Every step through the clinic workflow – scheduling, diagnostics, treatment, and billing – applies the same updated records and supports quality service delivery. It’s commonly implemented through the use of standardized data-sharing technologies like APIs as well as custom approaches. Forward planning helps tailor to specific functions and achieve successful integration within your organization.
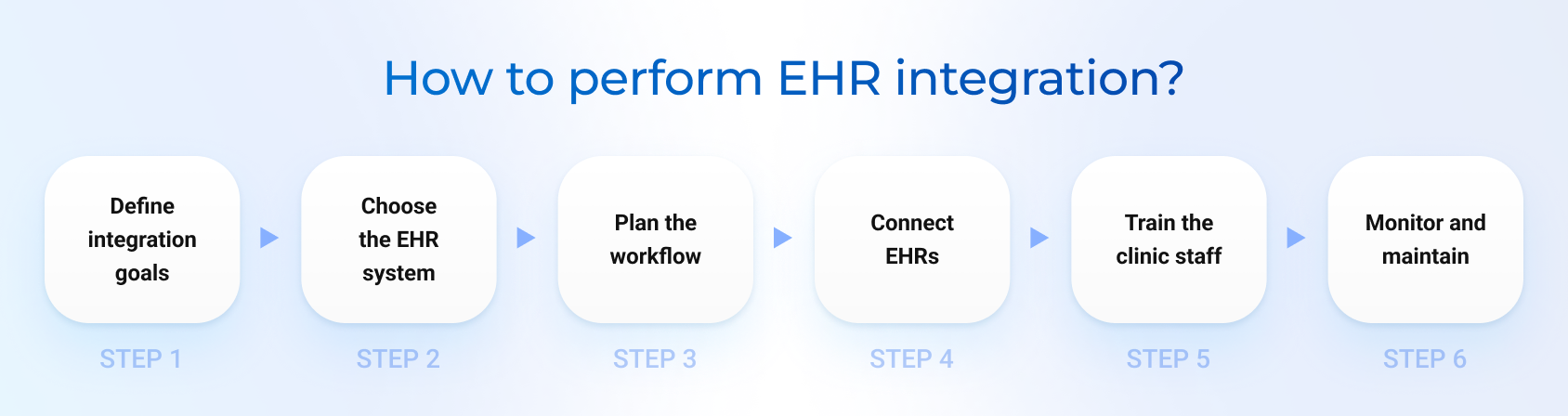
How to perform EHR integration?
The structured approach to integrating EHRs allows your facility to ensure a smooth transition and successful implementation. Here are the core steps to help you perform the integration effectively.
1. Define integration goals
Like with any other process, setting specific goals helps guide decisions and measure success throughout the integration process. Before the actual technical work, the clinic has to clearly outline what they want to achieve. As a rule, aims can refer to data accuracy, better interoperability, or other care-related tasks.
2. Choose the right EHR system
It’s a necessity to pick the solution that aligns with the current clinic’s operational needs and remains scalable for future growth. Your EHR system has to support integration with other tools you use or be part of advanced healthcare platforms with extended functionality. The efficient EHR integration has to support seamless data exchange between practitioners, labs, pharmacies, and other related apps.
3. Plan the integration workflow
It commonly involves creating a detailed roadmap for how chosen solutions will connect and what data will be shared. That’s especially essential for facilities that decide to complete the integration through standardized APIs or other protocols. The clinic needs to collaborate with IT teams, vendors, and medical staff to design its own workflow. At the same time, there is an opportunity to go with a ready-to-use solution like LinkHMS with a defined workflow to fit your clinic flow.
4. Connect EHRs
If you decide to handle technical implementation on your side, you continue working with the IT team to link EHRs to other solutions. It requires specific efforts to follow security protocols, manage data, and conduct various tests for smooth data exchange. With off-the-shelf solutions, this step takes less time and requires fewer resources to invest, as everything is handled by your provider.
5. Train your clinic staff
All users (doctors, nurses, administrative staff, lab workers, pharmacists) must be trained to use the integrated features when the necessary components are connected. Training focuses on improving their individual workflows and overall patient care. It’s recommended that separate documentation and guides be introduced for each user role, as their tasks vary and embrace different flow aspects.
6. Monitor and maintain
It’s hard to complete the integration without continuous monitoring and support. You always need to ensure everything runs smoothly. Regular performance checks, updates, and user feedback help identify issues early and keep operations aligned with your evolving clinic needs.
Breaking the complex process down into clear steps makes it easier to manage. You can save time, prevent errors, and make it work better for your healthcare practice.
Challenges of electronic health record integration
Healthcare providers need to be prepared for some challenges when connecting different software. As you understand possible obstacles, you can prepare and better undergo the overall integration process.
Data standardization
If the records are not consistent, data from one system can be confusing or even unreadable in another. It might lead to care delays, incorrect information, and extra work to fix the data manually. Therefore, EHR integration should embrace data standardization to use the proper formats, codes, and labels. Always ensure your healthcare solutions use the same medicine names, diagnosis codes, lab results, or prescription orders to navigate this data within healthcare environments.
Compatibility and interoperability between solutions
When we talk about integrating the EHR system with billing software, lab tools, and scheduling platforms, they might not be designed initially to communicate with one another. The lack of compatibility requires more effort through custom solutions or middleware to bridge the gaps. The difference in structure or technology approaches makes data exchange limited and unreliable. It’s necessary to involve IT experts to support proper integration and testing.
Compliance with privacy regulations
Healthcare data is extremely sensitive, so it must remain secure, encrypted, and only accessible to authorized users. The core integration aspects deal with setting up access controls, audit logs, and secure data transfer methods. Besides, all the implemented solutions need to follow strict security regulations like GDPR and HIPAA. Any failure to comply could cause legal issues, fines, and loss of patients’ trust.
High implementation costs
It’s a known fact that integration pays off in the long run through better efficiency and fewer errors. However, the initial investment can be a big challenge. The clinic’s budget should cover expenses on software licenses, customizing solutions, hiring IT experts, training staff, etc. It can be really hard to cover these expenses for clinics with limited budgets. Get prepared to face this challenge with accurate budget planning to avoid the expense increase due to unexpected changes.
Technical complexity
Strong technical support can prevent your facility from facing delays or failing integration altogether. The team puts special efforts into connecting healthcare workflows with the platform architecture. The common challenges are also related to technical tasks like mapping data correctly, preventing data loss, etc. Moreover, all implemented solutions need ongoing monitoring and maintenance to handle changes and updates in the clinic workflows.
As healthcare providers understand the possible obstacles, they plan better, avoid mistakes, and make smoother transitions. Challenges like data differences, technical issues, and high costs can be managed successfully with the right tools and support.
5 reasons to start EHR integration
The availability of the EHR system isn’t enough to fully and efficiently adopt it in medical practice. Connecting your EHR with other healthcare solutions can genuinely differentiate your clinic operations and unlock new levels of accuracy and connection.
Here are five compelling reasons why now is the right time to start integration with EHR systems.
Better patient care
Clinics can build connected healthcare environments by integrating EHRs with other systems for labs, prescriptions, or patient visits. It enables complete and up-to-date data about patients’ conditions, which leads to improved care. Even when the patient sees multiple speсialists or switches providers, practitioners don’t miss vital details, have relevant information, and make accurate decisions.
Time-saving workflows
EHR integration reduces repetitive tasks for medical staff due to system interoperability. There’s no need to enter varying clinical operations manually. Appointment time, invoices, medicine prescriptions, and test results all sync in real time. This kind of automation saves hours of admin work, shortens patient wait times, and allows practitioners to spend more time on direct patient care.
Fewer errors
Every time the clinic staff updates some health records, they are consistently shared across other modules. It doesn’t require manual data entry for separate software or related systems. Instead, it helps prevent medical errors, missing notes, or duplicated records. EHR integration lowers risks of mistakes and eliminates repeated tasks.
Improved communication
It’s a good reason to support better teamwork and quicker responses by implementing EHR integration solutions. When the practitioner reviews data like lab results, the moment they are ready, and other specialists follow the same care plan, the healthcare process manages to involve all the engaged parties. They work for coordinated care with access to patient information in real time.
Regulatory compliance
Healthcare facilities always deal with strict data privacy regulations and reporting standards. Accurate, secure, and complete EHRs help them stay compliant and manage records at the highest levels. Clinics get the opportunity to reduce legal and administrative risks while boosting trust with patients and regulators. It greatly supports easier reporting for insurance, audits, and public health tracking.
The decision to integrate EHRs is a smart move for any healthcare facility. If you want to stay competitive and improve care services, efficient data flow management should be among your top priority tasks.
Conclusion
Healthcare providers that make EHR integration a key focus invest in the right tools. It brings accuracy to patient care and creates smoother workflows. Real progress requires making an effort and addressing challenges, but this change is essential for the future of healthcare.
Would you like to find an efficient way to integrate Electronic Health Records (EHRs)?
Start with LinkHMS — our all-in-one hospital management system designed to make EHR integration fast, secure, and seamless. Built-in tools for patient record management, scheduling, invoicing, pharmacy, and lab coordination connect every part of your clinic in one place.
FAQs
What is EHR integration?
It’s a process of making medical records accessible across software solutions. The goal is to create a seamless flow of information to provide quality healthcare services.
How long does integration with EHR systems typically take?
The timeline depends on the complexity of the systems involved, chosen integrations, and the readiness of existing infrastructure. Simple integrations can take a few days, while more complex projects may require several months to complete.
How does it improve communication between departments and providers?
Integration enables real-time access to patient data across various departments and systems, ensuring that everyone involved in care has the most accurate and up-to-date information.